Who should get tested for Cocci? What tests should they receive? Learn more about the tests for Cocci.

DIAGNOSTIC TESTING
If you or someone you love has symptoms that are consistent with Cocci, you may want to know about testing. Who should get testing? Centers for Disease Control and Prevention recommend testing for anyone who lives in or who has traveled to the endemic area (Figure 1) and who has experienced one of the following:
Symptoms of community-acquired pneumonia while living in or having traveled to areas where Valley Fever is highly prevalent

Erythema nodosum after recent respiratory symptoms
Linked to a known outbreak

Symptoms of community-acquired pneumonia of unknown cause that has not responded to a round of antibiotics
Figure 1. Areas affected by Cocci. Reproduced with permission from CDC and MSGERC.

Advocate! Advocate! Advocate!
About 25% (1 in 4)
cases of community-acquired pneumonia in endemic areas are due to Cocci.
This is a lot of Cocci. With a one in four chance of developing Cocci, you would think testing would be common. Unfortunately, in several studies, less than 20% of people who had community-acquired pneumonia in an endemic area were tested for Cocci.
Why is this the case? It could be a number of factors—the clinicians aren’t thinking about it, they may not know what test to order, or they may think the disease will go away on its own. The point is you can ask to be tested if you meet the above criteria. The questions below may help you advocate for testing. If you’ve traveled to an endemic area and you becomes sick, it is even more important to advocate for yourself. Not all healthcare providers do a thorough travel or history or “think fungus” when evaluating pneumonia.
Who will order diagnostic testing?
Most healthcare providers can order diagnostic testing. In Arizona, you can even order your own laboratory testing, but you should work with a qualified healthcare professional to interpret the results. Here are some of the types of clinicians who can help you:
 Your primary care provider. Your primary care provider is most likely experienced in managing community-acquired pneumonia. This person can meet with you to go over the results of your testing and help you decide next steps.
Your primary care provider. Your primary care provider is most likely experienced in managing community-acquired pneumonia. This person can meet with you to go over the results of your testing and help you decide next steps.

Urgent care provider. Urgent care providers also see a lot of community-acquired pneumonia. They can also order the diagnostic tests. Ask how you will get your results and what happens after that.

Emergency room provider. If your symptoms are severe enough, you may be seen in the emergency room. The provider may order the test there or admit you if you are sick enough. Ask about how long the testing will take and when you will get results.

Pulmonologist. A lung doctor may see you if you have a severe lung problem or if x-rays show something unusual or abnormal in your lung. The spots on the lung caused by Cocci can be confused for lung cancer. So don’t be afraid to remind them to check for Cocci if you meet the criteria for testing.

Infectious Diseases Clinician. An infectious diseases doctor usually does not treat patients with community-acquired pneumonia, but you may be under their care for other health issues. Or your primary care provider may refer you to an ID clinician for a challenging case of pneumonia. The ID provider should be well-equipped to diagnose and manage your condition.

Oncologist. A cancer doctor may see you if you have a suspicious spot on your lung. The oncologist may be following you for cancer and notice a spot, or you may be referred to them because of an abnormal X-ray. About 5% of Valley Fever cases will develop a pulmonary spot (nodule). This could be confused for lung cancer, triggering a cancer workup. So don’t be afraid to remind your oncologist to check for Cocci if you have a suspicious spot on your lung and you have had or are at risk for the disease.
- Given my travel/residence history and my symptoms, could this be Valley Fever?
- What test will you order to check for Valley Fever?
- How is the test performed? Is it a blood draw?
- Will you do any imaging?
- Is there any reason to do any more invasive testing?
- What does the test measure?
- How soon will the results get back?
- How will the results be given to me (will you call me personally)?
- Will I require any additional testing?
- If the test is positive, will you refer me or treat me?
![]()
TESTING FOR COCCI
For Valley Fever
Blood (serology) tests
![]()
Enzyme-immunoassay (EIA) Serum Test for Antibodies
- Source: Blood
- What it’s testing for: Antibodies to Cocci
- Advantages: The test is relatively sensitive and can generally produce a quick yes/no answer
- Disadvantages: Not as specific as some other tests, so confirmation with a second test is often recommended
Immunodiffusion Serum Test for Antibodies
- Source: Blood
- What it’s testing for: Antibodies to Cocci, provides a qualitative result
- Advantages: The test is very specific and simple. More helpful for prognosis and disease management
- Disadvantages: Slow turn-around time; not as sensitive as the other tests, more helpful for prognosis and disease management
Complement fixation (CF) Serum Test for Antibodies
- Source: Blood
- What it’s testing for: Antibodies to Cocci, provides a quantitative result
- Advantages: The test is sensitive and can be used for measuring disease severity and progression
- Disadvantages: Slow turn-around time. more helpful for prognosis and disease management
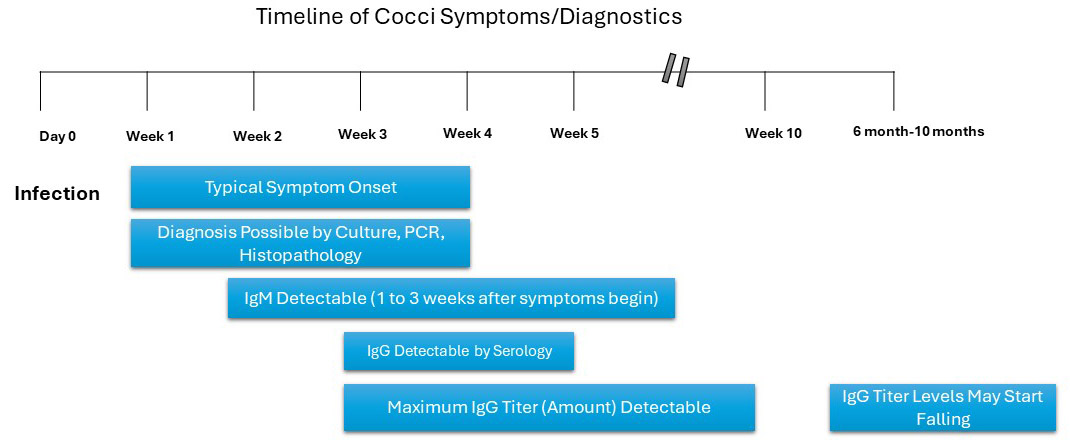
Timing of Tests
Your provider may need to repeat testing or use confirmatory testing to establish that you have Cocci. Figure 2 gives a snapshot of when tests tend to become positive or negative during the course of the disease. The Science Sidebar provides more detail about why some of the tests may be negative even if you do have Cocci. The bottom line is that your provider will most likely have to test you more than once.
Figure 2. Timeline of Cocci illness and when diagnostic tests are generally positive or negative. Modified from timeline provided by UC Davis.
1/3
or more patients with Valley Fever have negative serologic tests. This is why repeat testing is important!
Other tests
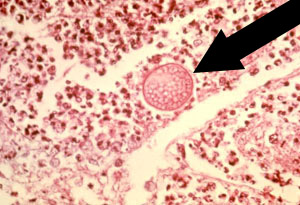
Microscopy/Histopathology (examination of tissues/cells)
This can be when the lab prepares slides from tissue, sputum, or a body fluid. The laboratory personnel can look for spherules as shown in Figure 3. This is not a very sensitive test, but when a spherule is found, it is considered very conclusive.
Figure 3. Arrow pointing to a Coccidioides spherule in lung tissue. This is a positive histopathology test. Reproduced from CDC website.
Fungal culture:
This is when the lab attempts to grow fungus from body tissue, sputum, or a body fluid, as shown in Figure 4. If the Coccidioides species is isolated, that is definitive evidence of infection. However, culturing is difficult because it has to be conducted on sputum or on tissue. Processing requires a specialized safety laboratory.
Figure 4. Cocci in culture: Showing white, cottony mold

Polymerase Chain Reaction:
(PCR) testing is a molecular test. This is only performed at some institutions as a research test, and it can only be used on sputum or tissue.
Imaging:
 X-ray imaging and computed tomography (CT)
X-ray imaging and computed tomography (CT)
Imaging is often used to diagnose community-aquired pneumonia. Your provider may use imaging (Figures 5 and 6) along with other tests such as serology and microbiologic tests in diagnosing Cocci.
For patients with complicated pulmonary Cocci, imaging can be helpful for diagnosis. This includes:
- Pleural effusion. The accumulation of fluid between the lungs and the tissues that line the lung and chest. of cases
- Nodules. Small clumps of cells in the lung, which are visible on imaging, as shown in Figure 6
- Cavitary lesions. These are nodules, masses, or consolidated areas of the lung that have an area of air in them (like a donut) Cavitary lesions can occur in 5-15% of cases. The cavitary lesions contain Coccidioides. Rupture of the cavitary lesions occurs in 2-4% of cases and can cause an empyema
- Empyema. A collection of pus in the cavity between the lung and the membrane (pleura) that surrounds it
Figure 5. X-ray image showing pulmonary Cocci. Image courtesy of Neil Ampel, MD.
Figure 6. Residual nodule from Cocci as seen on CT scan. Image reproduced with permission from UC Davis Health.

Skin Testing:
 Skin testing is used to determine if you have had an immune response to Coccidioides. It is similar to the skin test for tuberculosis—you get a small injection on the inside of your forearm—if a bump forms, it is positive. A positive test generally means that you are immune to Cocci and will not get Valley Fever in the future. However, some people with immunodeficiency don’t mount an immune response and so they may test positive even if they have already been exposed to Cocci .
Skin testing is used to determine if you have had an immune response to Coccidioides. It is similar to the skin test for tuberculosis—you get a small injection on the inside of your forearm—if a bump forms, it is positive. A positive test generally means that you are immune to Cocci and will not get Valley Fever in the future. However, some people with immunodeficiency don’t mount an immune response and so they may test positive even if they have already been exposed to Cocci .
For Disseminated Disease
When disease disseminates, it can mimic many other diseases. Therefore, the diagnosis can be challenging. Accurate diagnosis requires a multidisciplinary approach. At this point, it is best to consider working with a specialist in a center that treats a lot of Cocci.
Here are some of the tests that may be involved:
Skin Involvement
If your healthcare provider suspects you have disseminated Cocci to the skin, they will most likely conduct serologic testing. This can include CT testing, which gives a quantitative measure (titers) of your immune response. The titers can become negative later in the disease course. Most likely, a skin biopsy will also be performed for culture and histopathology. This is because the serology may not be helpful, particularly in immunocompromised patients.
Joint/bone involvement
If joint pain is involved, your healthcare provider will need to determine if there is bone involvement alone or it has progressed to adjacent structures such as joints, tendons, or other soft tissues.
Typically a biopsy will be obtained. This might involve percutaneous biopsy, CT–guided needle biopsy, or surgical removal. For joint involvement, joint fluid can be obtained by arthrocentesis. Serologic testing, particularly the CF titer, will help monitor the disease.
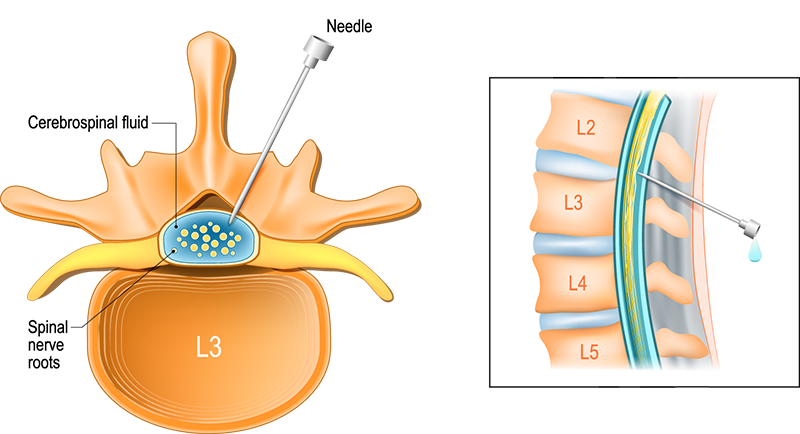
Central Nervous System (CNS) Involvement
For a patient with suspected CNS dissemination, a lumbar puncture (spinal tap) must be performed. As shown in Figure 7, this involves inserting a needle in the lower back to access the thecal sac, which contains the cerebrospinal fluid surrounding the spinal canal. Using this method, your provider can sample your spinal fluid and measure pressure, and cell counts, including the presence of eosinophils, glucose, and Cocci antibodies. A CSF culture and serologic testing will also be performed. A CT scan of the brain without contrast is important and can help identify high pressure (hydrocephalus) in the brain. A magnetic resonance imaging (MRI) test might be needed to look for specific brain problems involving blood vessels and other soft tissue structures. Some providers recommend that all patients with Cocci get a brain MRI early in the disease course as a baseline.
Figure 7. Diagram illustrating the lumbar puncture process.