Who should get tested for aspergillosis? What tests should they receive? Learn more about the tests for aspergillosis.

DIAGNOSTIC TESTING
Who Gets Sick and Who Should Get Tested?
When we think about testing for aspergillosis, it’s helpful to recall who is at risk for allergic, chronic, or invasive forms.
For the allergic forms, recall that we are most concerned with patients with asthma and cystic fibrosis. However, sometimes people don’t fit the usual profile, Therefore, when there is evidence of lung infection on a chest x-ray or computed tomography (CT) scan, symptoms and high serum igE levels, and a lack of response to antibiotics, the doctor may start testing for allergic aspergillosis. People who have chronic lung conditions like emphysema or tuberculosis are at risk for the chronic forms of aspergillosis. For invasive forms, people with immunocompromising conditions or occasionally severe influenza or COVID-19 are at risk.
People who need testing are those who have symptoms consistent with a particular type of aspergillosis. The healthcare team will take a careful medical history, review symptoms, and evaluate other potential causes of those symptoms. For instance, people suspected of having chronic pulmonary aspergillosis would warrant testing when they have three months of symptoms.
Does this mean everyone who “has” Aspergillus in their body is going to get sick? No, it does not. This distinction gets tricky from a diagnostic standpoint. See the Science Sidebar on Aspergillosis: When the Aspergillus Colony Invades to learn more.
The tests used to diagnose aspergillosis vary for allergic vs infectious forms. Both are described below. Note that this content is based on testing in adult patients; see our forthcoming primer on infections in pediatric patients.
Diagnostic Tests for Allergic Forms of Aspergillosis
Complete blood count 
- Source: Blood
- What it’s testing for: Increased levels of eosinophils
- Advantages: Easy test
- Disadvantages: The eosinophil levels are not always elevated in all cases of allergic aspergillosis.
Aspergillus immunoglobulin E levels.
- Source: Blood
- What it’s testing for: Antibodies to Aspergillus of the subtype E (IgE), a marker of the allergic response to Aspergillus
- When it is used: To diagnose ABPA and Chronic Pulmonary Aspergillosis
- Advantages: Helpful for diagnosis and for monitoring how well you are responding to therapy
- Disadvantages: Testing is for specific Aspergillus species (e.g., fumigatus vs niger).
Imaging

- Source: Potential affected body part that will be imaged
- What it’s testing for: Images consistent with ABPA. A chest x-ray (or computed tomography [CT] scan) can pick up ABPA 50% of the time.
- Advantages: Relatively easy to obtain
- Disadvantages: Doesn’t always pick up every case.
Allergy Skin Testing
- Source: Testing on Skin. A small amount of A. fumigatus is put under your skin to see if there is swelling and itching (which is consistent with an allergic reaction)
- What it’s testing for: Immune response to Aspergillus (IgE antibodies)
- When it is used: Diagnosing ABPA
- Advantages: Not very invasive, can give results quickly
- Disadvantages: The test is less sensitive (misses some cases) as compared with the blood IgE test.
Histopathology

- Source: Mucus from patients with nasal polyps (in the setting of a positive IgE blood test or skin-prick test)
- What it’s testing for: To find evidence of the fungi in the mucus
- When it is used: Diagnosis of allergic fungal rhinosinusitis
- Advantages: More sensitive that fungal culture of nasal secretions and relatively quick
- Disadvantages: Requires expert reviewer.
Diagnostic Tests for Invasive Forms of Aspergillosis
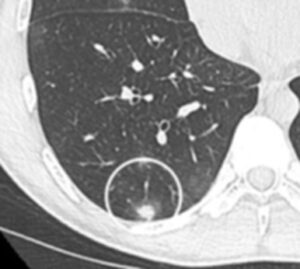
Healthcare providers will think about invasive aspergillosis in sick people who have aspergillosis risk factors. They will also look for imaging results consistent with invasive aspergillosis (Figure 1). So a lot of the time the clinical signs (sickness) and the radiologic (imaging) signs are the trigger for performing microbiologic testing.
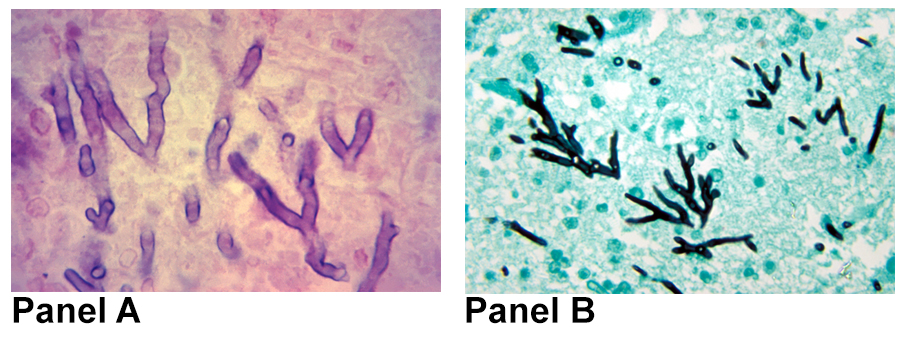
The gold standard diagnostic tests for invasive aspergillosis are culture and histopathology. For a fungus to be “proven,” the provider relies on tests performed on a sample from a site that is not normally contaminated with fungi (i.e., sterile). That sample would need to grow fungus when put in culture (Figure 2). Alternatively, for a proven case of aspergillosis, a sample of tissue needs to show invasive aspergillosis on histopathology (Figure 3). These tests are described in more detail below.
One issue with these gold-standard tests (histology and culture) is that they are a bit invasive—they usually require a biopsy or at least a procedure. Many of the patients with invasive aspergillosis can be medically fragile, so it’s a balancing act when considering these tests vs the problems they may cause.
Imaging (Xray and CT are both recommended for testing for invasive aspergillosis)
- What it’s testing for: Imaging consistent with invasive aspergillosis
- Advantages: Relatively easy to obtain, part of the diagnostic picture
- Disadvantages: These results are not specific—bacterial infection in the lung can look similar to fungal infection in the lung, for example. This doesn’t always pick up all cases (particularly in patients who are not immunocompromised); some of the features could be caused by another disease (e.g., other mold infections).
Figure 1. CT of the lung of an immunosuppressed patient shows a nodule in the right lower lobe of the lung (circled area). This shows the halo sign, in which there is a solid part surrounded by a small, ground-glass-looking area that is the halo. Reproduced from Wikimedia Commons. Article authors: Annemie Snoeckx, Pieter Reyntiens, Damien Desbuquoit, Maarten J. Spinhoven, Paul E. Van Schil, Jan P. van Meerbeeck, Paul M. Parizel, CC BY 4.0 <https://creativecommons.org/licenses/by/4.0>, via Wikimedia Commons.
Fungal Culture
- Source: Respiratory samples, sinus samples, and tissue taken as a biopsy from other body regions where invasive aspergillosis is suspected (eg. skin biopsy)
- What it’s testing for: The presence of live fungi that can grow in culture
- When it is used: Testing for invasive aspergillosis in the particular body region
- Advantages: Helps definitively establish invasive aspergillosis when obtained from a sample in a site that is normally sterile (not normally contaminated with fungi). Aspergillus is considered a fast grower and often the fungus can be seen within three days.
- Disadvantages: Not all sites are sterile; for example, respiratory samples yielding positive culture may reflect contamination rather than invasive disease. A confirmatory test may be required. Finally, some samples that contain Aspergillus fail to grow fungus in culture, so the test is not very sensitive.
Histopathology
- Source: Samples from the respiratory tract, sinuses, or other body regions where invasive aspergillosis is suspected
- What it’s testing for: Evidence of Aspergillus invading tissue when the sample is looked at under a microscope. This could be visualized as the finding of acute-angle branching, septate hyphae (Figure 2) and signs of tissue damage.
- When it is used: Testing for invasive aspergillosis in the particular body region (presence of hyphae) as well as evidence of damage to the tissue
- Advantages: Helps definitively establish invasive aspergillosis
- Disadvantages: This test does not always pick up all cases of invasive aspergillosis. In addition, the appearance of fungi under the microscope can be confusing. For example, other molds might look like Aspergillus. It’s important to interpret histopathology in conjunction with culture and other tests.
Figure 2. Image showing fungus growing in a culture as fungus balls. This particular sample was taken from the vitreous, which is part of the eye. This patient was diagnosed with invasive aspergillosis. [Permission Pending]
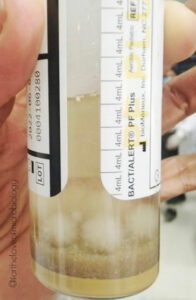
Figure 3. (Panel A) Microscopic image of Aspergillus hyphae present in a human lung specimen. Panel B shows the microscopic image of brain biopsy tissue that shows Aspergillus hyphae in the brain. Aspergillus hyphae are known to branch in acute angles (less than 90 degrees) and have division (septa) in their hyphae. Reproduced from the CDC/Armed Forces Institute of Pathology https://phil.cdc.gov/FAQ.aspx or https://phil.cdc.gov/Details.aspx?pid=4228
Non-culture-based tests
Other tests are also used for diagnosis of Aspergillus. While these tests are not as definitive as culture or histopathology, they can generally be performed more quickly and with less invasive measures.
Galactomannan (GM) antigen test (via enzyme immunoassay, GM-EIA)
- Source: Blood or bronchoalveolar lavage (BAL) fluid
- What it’s testing for: A polysaccharide (sugar) that makes up part of the Aspergillus cell wall. The test is performed using a process called EIA in the laboratory. In some cases, it is also tested with a lateral flow assay in a point-of-care test (like a COVID-19 test or a pregnancy test).
- Advantages: Galactomannan is easy to measure in serum. It provides a quantitative result, so it is useful for monitoring response to treatment over time.
- Disadvantages: The test is not very sensitive. Rarely, exposure to certain substances can cause a false positive. The test can also cross-react with some other fungi, including Penicillium and Histoplasma fungi.
Beta-D-glucan
- Source: Blood or cerebrospinal fluid
- What it’s testing for: A polysaccharide (sugar) found in fungi. The Beta-D-glucan test is not specific for Aspergillus.
- Advantages: Beta-D-glucan is easy to measure in serum. It provides a quantitative result, so it is useful for monitoring levels over time. It also has a quick turnaround time, so it can be used to guide decision making.
- Disadvantages: The test is very unreliable for establishing aspergillosis. The test has low specificity for Aspergillus. There are a lot of false positives with the test. It is often positive with many other fungal infections, when certain medications such as intravenous immunoglobulin are prescribed, or when dialysis filters are used.
Polymerase Chain Reaction
- Source: Blood, and BAL fluid
- What it’s testing for: Aspergillus DNA in the tissue
- Advantages: PCR is specific Aspergillus and can actually determine both the genus and species. It can also identify changes in the Aspergillus DNA that are associated with resistance to certain therapies.
- Disadvantages: PCR testing is not completely standardized yet in the United States. There are only a few commercially available assays, so is not readily available in many centers.
Metagenomic Next-Generation Sequencing
- Source: Blood
- What it’s testing for: The presence of fungal DNA outside of cells (microbial cell-free DNA). Next-generation sequencing provides a readout of thousands of infectious agents in one blood test.
- Advantages: The test is relatively non-invasive, quick, and specific. It can also identify co-infections.
- Disadvantages: The test has not been extensively studied and validated against other fungal tests in large groups of patients.
Clinical Trials and Investigational Diagnostics
In the area of Aspergillus diagnostics, there is interest in less invasive and point-of-care testing.
One of the most promising areas of investigation is the use of breath diagnostics for fungal disease. With breath testing, clinicians propose that individual fungal species and different stages of the disease will have specific recognizable profiles in the patient’s breath. Read a review article to learn more about this convenient and non-invasive test for fungal disease.
Urine testing is also appealing because it is less invasive than a blood draw of a BAL. Dipstick type point-of-care tests (like are used in pregnancy) are being investigated.
Frequently Asked Questions
This is a great point. Sometimes it is very hard to tell the two apart. Aspergillus in the lung can look like a lung tumor, and aspergillosis can “spread” to the brain or other parts of the body like a cancer would. That’s where diagnostics become very important. Suspicious spots will most likely need to be biopsied to determine if the illness is caused by cancer or an infection like Aspergillus and to establish the right treatment.
- Why do you suspect aspergillosis?
- What test will you order to check for aspergillosis?
- How is the test performed? Is it a blood draw? Or something more invasive?
- Will you do any imaging?
- What does the test measure?
- How soon will the results get back?
- Might you require additional testing?
- What happens if the test is positive for Aspergillus?
![]()