Who should get tested for invasive candidiasis? What diagnostic tests should they receive? Learn more about the tests for invasive candidiasis.

DIAGNOSTIC TESTING
Who Gets Sick and Who Should Get Tested?
Invasive candidiasis is a serious fungal infection, and studies show that when therapy is started early, patients do better, so early diagnosis is important. However, the symptoms associated with Candida are not very specific and can be associated with other infections, such as bacterial infections.
For these reasons, healthcare providers often start treatment early for patients who are at high risk for invasive candidiasis or who have symptoms and have not responded to antibacterial drugs. This means they are starting treatment before they have diagnostic results. However, more often, they will confirm Candida with testing even after they have started therapy. Diagnostic tests for invasive candidiasis are discussed below. See the TREATMENT OF INVASIVE CANDIDIASIS section to learn more about treatment strategies.
We’ve talked about Candida normally being on our skin and the lining of our gut (a term called colonization). With C. auris, we want to know if it’s colonizing the skin because it’s contagious. But for most other forms of Candida, we are only concerned when it is causing a problem (invasive candidiasis). That’s why we typically test for invasive candidiasis from sterile sites.
Tests for Candida auris Colonization
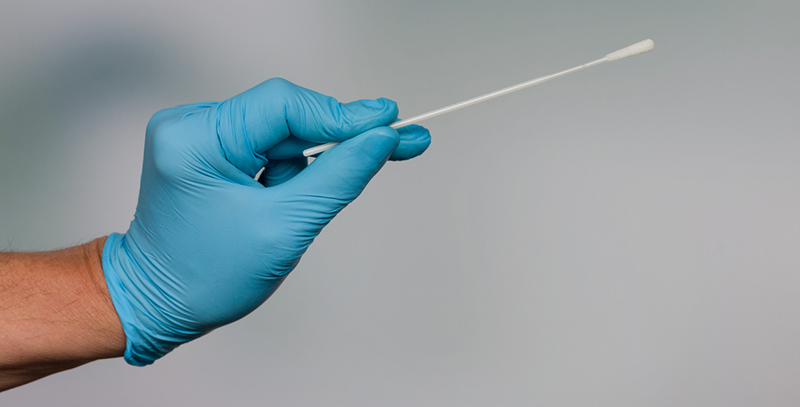
As mentioned, because Candida auris is so easily spread, it’s important to determine if patients who have been exposed to C. auris are colonized (carrying) the fungus. This allows healthcare providers to take precautions to prevent the spread to other people and to watch the colonized person closely given they may develop invasive disease.
- Source: Swabs of the armpits and groin
- Advantage: Doesn’t miss cases or frequently label negative cases as positive.
- Disadvantage Requires 2-7 days, depending on the test type.
- How the Test Impacts Decision Making: The test is sent away for analysis. If the patient is at high risk for C. auris, they may be treated with extra infection and control precautions such as placing them in a single room and special care after contact while waiting for the test results to come back. If the test shows the patient is colonized, they would be treated with all the same precautions a person with an infection would receive.
Diagnostic Tests
Healthcare providers will test for invasive candidiasis in patients who have risk factors and who are sick. The treatment section goes into more detail about when providers will start therapy in different approaches.
Before we get into the details of testing, it’s helpful to think about three types of invasive candidiasis: candidemia alone, candidemia plus deep-seated candidiasis, and deep-seated candidiasis alone, as shown in Figure 1. In some settings, these groups are about equal in size. But it’s important to recognize that blood cultures will not pick up all the cases of deep-seated candidiasis. This is something to keep in mind when reviewing diagnostic test results.
Figure 1. The types of invasive candidiasis that can be present. Note that in the cases of deep-seated candidiasis, the infection will not be present or detectable in the blood in a large proportion of cases. Adapted from Clancy, Clin Infect Dis. 2013;56:1284-1292.

TESTS FOR YEASTS/CANDIDA
We can think of these tests as those that help us establish that a yeast is present. That’s the first step.
![]() Fungal Culture
Fungal Culture
- What it is testing for: The presence of live fungi that can grow in culture
- When it is used: Testing for invasive candidiasis in the particular body region
- Advantages: Helps definitively establish invasive candidiasis when obtained from a sample in a site that is normally sterile (not normally contaminated with fungi). Culture is also needed for antifungal susceptibility testing, which is an important factor when considering the therapy to provide.
- Disadvantages: The test is relatively slow—it can take about two to three days or more for Candida to grow in a blood culture. It also misses some cases. For example, a blood culture can miss approximately 50% of cases of deep-seated candidiasis . So, the test is not very sensitive.
Histopathology
 Source: Biopsy or needle-aspiration from the normally sterile site
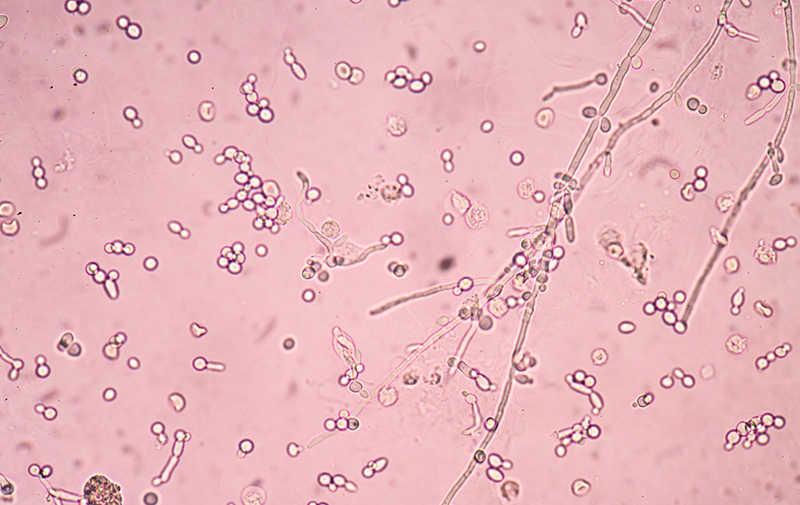
Source: Biopsy or needle-aspiration from the normally sterile site- What it’s testing for: Evidence of Candida in the sample. Figure 2 shows Candida under the microscope.
- When it is used: Testing for invasive candidiasis in a particular body region
- Advantages: Helps definitively establish invasive candidiasis, Use of special stains specific for Candida can help.
- Disadvantages: The test is relatively insensitive. Also, a biopsy might be difficult for a medically fragile person. Finally, sometimes the site can be colonized with Candida, making it hard to tell colonization from an actual invasive infection.
Figure 2. Candida under the microscope. The image shows the budding forms of Candida as well as the tubular hyphae.
Non-culture Based Tests
Other tests are used for the determination of whether fungi, yeasts, or Candida are present.
Beta-D-Glucan
- Source: Blood
- What it’s testing for: A polysaccharide (sugar) found in fungi. The Beta-D-glucan test is not specific for Candida.
- Advantages: Beta-D-glucan is easy to measure in serum. It also has a quicker turnaround time than blood cultures, so it can be used to guide decision making. It has relatively good sensitivity. The test can be used together with other tests to increase confidence in the results. It can also be followed over time in patients who are at high risk for candidiasis.
- Disadvantages: There are a lot of false positives with this test. It is often positive with many other fungal infections, when certain medications such as antifungals or intravenous immunoglobulin are prescribed, or when dialysis filters are used.
Polymerase Chain Reaction (PCR)
- Source: Blood or other sample (fluid from the abdomen area, etc.)
- What it’s testing for: Candida DNA in the sample
- Advantages: PCR is specific. It can actually determine both the genus and species of Candida. It can also identify changes in the Candida DNA that are associated with resistance to certain therapies. Some PCR tests can identify organisms very rapidly and can be performed on whole blood.
- Disadvantages: PCR testing is not completely standardized yet in the United States. There are only a few commercially available assays, so is not readily available in many centers. A specialized machine for PCR testing on blood is not available in all facilities. Finally, since PCR tests are typically set up to test for the most common Candida species, some of the rarer species can be missed.
Metagenomic Next-Generation Sequencing
- Source: Blood
- What it’s testing for: The presence of fungal DNA outside of cells (microbial cell-free DNA). Next-generation sequencing provides a readout of thousands of infectious agents in one blood test.
- Advantages: The test is relatively non-invasive, quick, and specific. It can also identify co-infections.
- Disadvantages: The test has not been extensively studied and validated against other fungal tests in large groups of patients. It is not widely available and can be costly.
Tests to Determine the Candida Species and Antifungal Susceptibility
With Candida infections, it’s important to figure out what the species is and any resistance patterns. This is very important, because a lot of decision making regarding therapy requires knowing the species of Candida.
Subculture
- Source: Specimen obtained from a culture
- What it’s testing for: The specific species of Candida and antifungal susceptibility
- Advantages: Gold standard for determining the species. For problematic samples, reference laboratories are very good at performing these traditional microbiologic tests.
- Disadvantages: Requires a sub-culture and is relatively slow (takes additional time).
Matrix-assisted laser desorption/ionization-time of flight (MALDI-TOF)
- Source: Positive blood culture
- What it’s testing for: Candida species and antifungal susceptibility testing through analysis of protein patterns for different organisms
- Advantages: MALDI-TOF is a sensitive, efficient and simple test. It requires only a small sample and has a reduced time to identification (saving approximately 24-48 hours) vs traditional microbiologic tests.
- Disadvantages: The cost of the machine for the test is relatively high. It works better with fresh samples. Identification relies on matching the output to databases for comparison. Therefore, if the database is out of date, the test can be inaccurate. This happens sometimes with C. auris, where new strains appear over time.
Frequently Asked Questions
That’s an important question. Many of the risk factors for invasive candidiasis are also risks for bacterial infections, so the populations overlap. In addition, many of the symptoms associated with invasive candidiasis (e.g., fever and chills) can also occur with bacterial infections. Your team should test for bacterial infections and treat them appropriately. Often, if a patient remains sick after treatment for a bacterial infection, it’s a sign that the underlying cause might be fungal.
Yes, some of the more traditional systems for studying yeasts misidentify Candida auris as other Candida species, such as Candida haemulonii. According to the CDC, the community is getting better at identifying C. auris, but misidentification is still a possibility. For more information about C. auris misidentification, see the CDC resource.
- Why do you suspect invasive candidiasis?
- What test will you order to check for invasive candidiasis?
- How is the test performed? Is it a blood draw? Or something more invasive?
- Will you do any imaging?
- What does the test measure?
- How soon will I get my results back?
- Might I require additional testing?
- Will you wait for the results of the test to start antifungal therapy? Why or why not?
- What happens if the test is positive for invasive candidiasis?
![]()